The role of stomach acid in depressive symptoms is an interesting one– while it’s hard to argue against the fact that the food we eat and our overall nutrition has an impact on our mental health, most individuals don’t really think about how it’s not just the food we eat, but about how we digest and breakdown this food, that plays a vital role in the function (or dysfunction) of key neurotransmitters, which dictate our emotions.
Low stomach acidity, or having a less acidic/more alkaline environment in the stomach, has not been receiving its due attention in popular health discourse. Having an acidic stomach environment is incredibly important to how we break down and absorb nutrients from our food– if our pH isn’t low enough, instead of deriving and utilizing essential vitamins and minerals found in our food, food particles of inappropriate sizes make way through our digestive system, wreaking havoc on the lining of our small and large intestines. When fats or protein particles damage the villi and microvilli that line our intestines, it overwhelms our immune system and triggers inflammatory responses. Unattended, this imbalance can lead to chronic digestive diseases like IBS (irritable bowel syndrome), GERD (gastroesophageal reflux disease), or Crohn’s disease.
But back to mental health– how does poor stomach acid balance contribute to depressive symptoms?
Role of Stomach Acid in Depressive Symptoms
I tread careful waters with my language here, because there is insufficient proof that low stomach acidity causes depression– depression is a complex mental health condition, with multiple factors at play, depending on one’s bioindividual makeup such as age, sex, environment, and genetics. But I can state with confidence that malnutrition has an impact on the way neurotransmitters are synthesized, worsening depressive symptoms in individuals who are already at-risk.
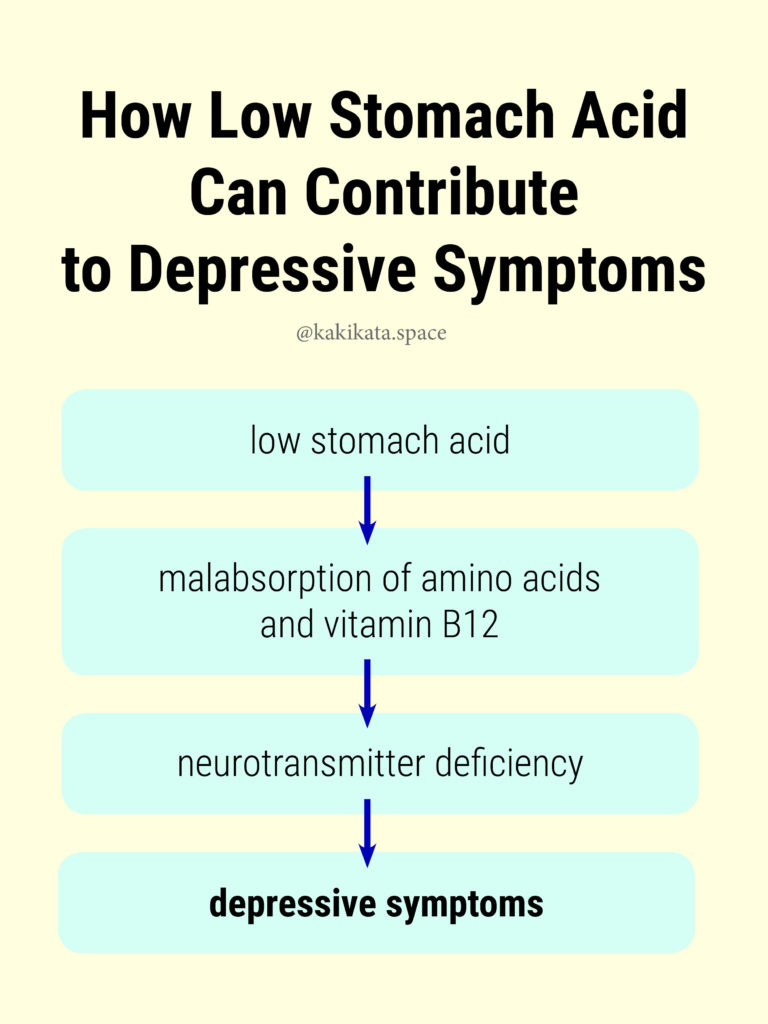
Amino Acids: Most neurotransmitters are built using amino acids by nerve cells. For example, the amino acid phenylalanin and tryptophan are processed by neurons to synthesize the neurotransmitter serotonin, also known as one of the “happiness” neurotransmitters, for its ability to elevate our mood.
If we have low stomach acid, we suffer from improper breakdown of protein and malabsorption of essential amino acids which serve as building blocks for neurotransmitters. With reduced absorption of amino acids, our bodies are led to neurotransmitter deficiency, as there is nothing to synthesize the neurotransmitters with. Subsequently, when we lack mood-elevating neurotransmitters like serotonin, we are led to depressive symptoms (Wright 2001).
Vitamin B12: In a similar vein, low stomach acidity means that our bodies might not be deriving important vitamins in adequate quantities. In particular, vitamin B12 plays a critical function in building and metabolizing neurotransmitters. Unsurprisingly, vitamin B12 deficiency has been correlated with depression in multiple observational studies– an interesting case study illustrates a patient who was treated with antidepressant and antipsychotic medication for months, before being checked for any nutritional deficiencies. The woman suffered from lethargy and excessive crying for years, but within two months of B12 treatment she returned to her baseline level of mood, with no follow-up treatment required (Berry, Sagar, and Tripathi 2003).
In this way, we can be eating a perfect, whole foods-based diet with plenty of protein, but still be left amino acid or nutrient deficient. Our bodies can only undergo the proper breakdown and absorption of food within a very narrow range of acidity, or about 1.5 – 3.0. Another reason why someone who is eating perfectly well finds that their eating habits have no impact on the way they feel– it’s not that their bodies aren’t responding well to proper nutrition, but it’s because the nutrients aren’t even being properly derived from the food.
By understanding how nutrition plays a vital role in the synthesis of emotion-lifting neurotransmitters such as serotonin, we can connect our digestive function with our mental health. While the science is still new and it’s not possible to determine that low stomach acidity will cause depression, considering that digestive dysfunction can contribute to depressive symptoms is important when we look to manage and take care of our own health.
What You Should Know About Stomach Acid:
Symptoms of Low Stomach Acidity
- Common symptoms include bloating, gas, heartburn, or acid reflux– while many individuals may brush these off as minor inconveniences, they can be symptoms of a serious digestive issue that needs to be addressed.
- Other symptoms: muscle cramping, diarrhea, constipation, food allergies or sensitivities, fatigue, acne, hair loss and brittle nails (often the case for women).
Causes
- Chronic stress— Because digestion is not essential when it comes to immediate survival, stress causes the body to divert blood away from digestive function and instead send itself to our muscles and brain. The decreased blood flow causes the production of digestive enzymes and juices to decrease, leading to low stomach acidity over time.

This is one of the reasons why I find adequate rest and meditative techniques to relieve stress to be very key to long-term health: it’s not just that leading a well-rounded life sounds great, but leading a well-rounded lifestyle is directly important to our physical and mental health.
- Antacids or medications for acid reflux and heartburn— These medications are often prescribed to neutralize acid, but they only prolong the issue of low stomach acidity. By continually taking them, we make our stomach environment less acidic, less able to break down and absorb nutrients, and cause further inflammation leading to digestive issues.
- Surgery— Certain surgeries can impact the way our gut produces enzymes. For example, gastric bypass surgery can reduce the amount of acid our stomach produces, leading to lower acidity.
The Key Takeaway
In this way, we should be looking at mental and physical health as interconnected systems. The role of nutrition and food to our mental health should not be trivialized; not just the food we eat, but how our bodies breakdown and digest the food we eat deserves just as much attention.
If we are suffering from depressive symptoms that we believe are caused by malabsorption, we can’t just be popping supplement and vitamin tablets in hopes that our nutrient uptake will be sufficient, but we must address deeper issues related to our digestive system. This means paying attention to our bodies for symptoms, addressing stress, resting adequately, and trusting that a balanced whole food-based diet can support our long-term health.

***
If you believe you may suffer from low stomach acidity and would like some more guidelines as to how to address it, you can read my article here [insert kakikata link] or shoot me an email at kokumura@kakikata.space for a more personalized recommendation! I also just enjoy receiving messages from people who find my material useful, and would love to hear from you– I read and respond to every email I get!
Kind regards,
Kaki
Source:
- Wright, Jonathan V. MD & Lenard, Lane Ph.D. (2001). Why Stomach Acid Is Good for You: Natural Relief from Heartburn, Indigestion, Reflux and GERD. M. Evans & Company.
- Berry, N. , Sagar, R. and Tripathi, B. M. (2003), Catatonia and other psychiatric symptoms with vitamin B12 deficiency. Acta Psychiatrica Scandinavica, 108: 156-159. doi:10.1034/j.1600-0447.2003.00089.x